Learn how a leading East Coast Health System boosted VA claim reimbursements by leveraging advanced technology and deep VA expertise via their revenue cycle partner, EnableComp.
The challenge
For over a century, a prominent non-profit health system on the East Coast has been a cornerstone of community health, employing more than 14,000 across several hospitals, physician practices, and outpatient facilities. Integral to its mission is providing exceptional care to all, including the veterans it serves. Veterans Affairs (VA) claims are a small, yet vital portion of the provider’s revenue stream.
The health system faced mounting challenges managing VA claims that threatened its ability to serve this important population effectively. The complexity of VA payer and authorization requirements overwhelmed in-house revenue cycle staff, resulting in prolonged processing times and an unsustainable number of written-off claims.
The health system recognized the need for a strategic partner with unmatched proficiency in VA revenue cycle management.
The solution
EnableComp developed a comprehensive strategy to revitalize the health system’s approach to VA claims, managing VA claims from initial claims submission all the way through final payment with a focus on yield
enhancement.
A dedicated team of VA revenue specialists was assigned to the health system. This team brought deep expertise in navigating the complexities of VA claims, including the nuances of different VA payers and authorization protocols.
Central to this performance turnaround was the role played by EnableComp’s proprietary e360 RCM® platform — the most advanced intelligent automation technology for the complex revenue cycle in the industry.
E360 RCM’s built-in reimbursement modeling was used to accurately project potential revenues, while automated denial management swiftly addressed issues that previously led to lost reimbursements. The platform’s underpayment identification system uncovered discrepancies that had gone unnoticed, ensuring the health system received the full reimbursement for care delivered.
EnableComp’s tailored solutions streamlined processes, reduced overhead, and recovered lost revenues, strengthening the health system’s financial foundation. This collaboration demonstrates how specialized expertise and advanced technology can resolve complex revenue cycle challenges, ultimately enhancing the health system’s capacity to serve veterans more effectively.
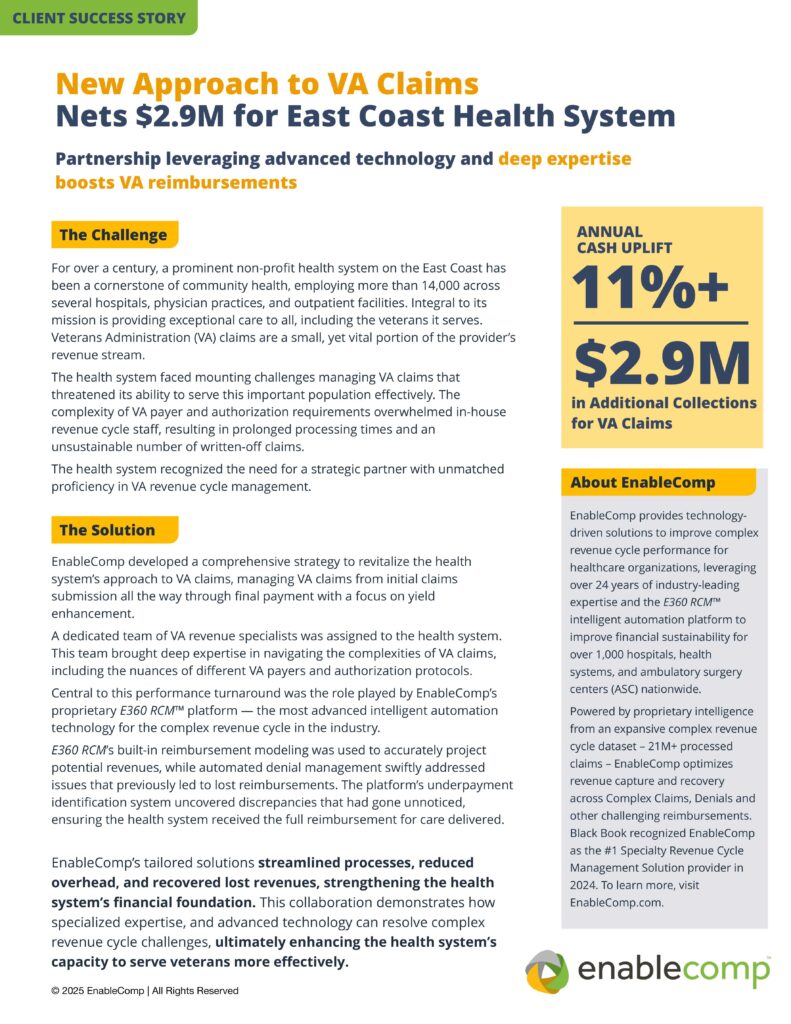
The bottom-line impact
The health system recovered $2.9 million in additional VA claim reimbursements and achieved an 11% annual cash uplift.