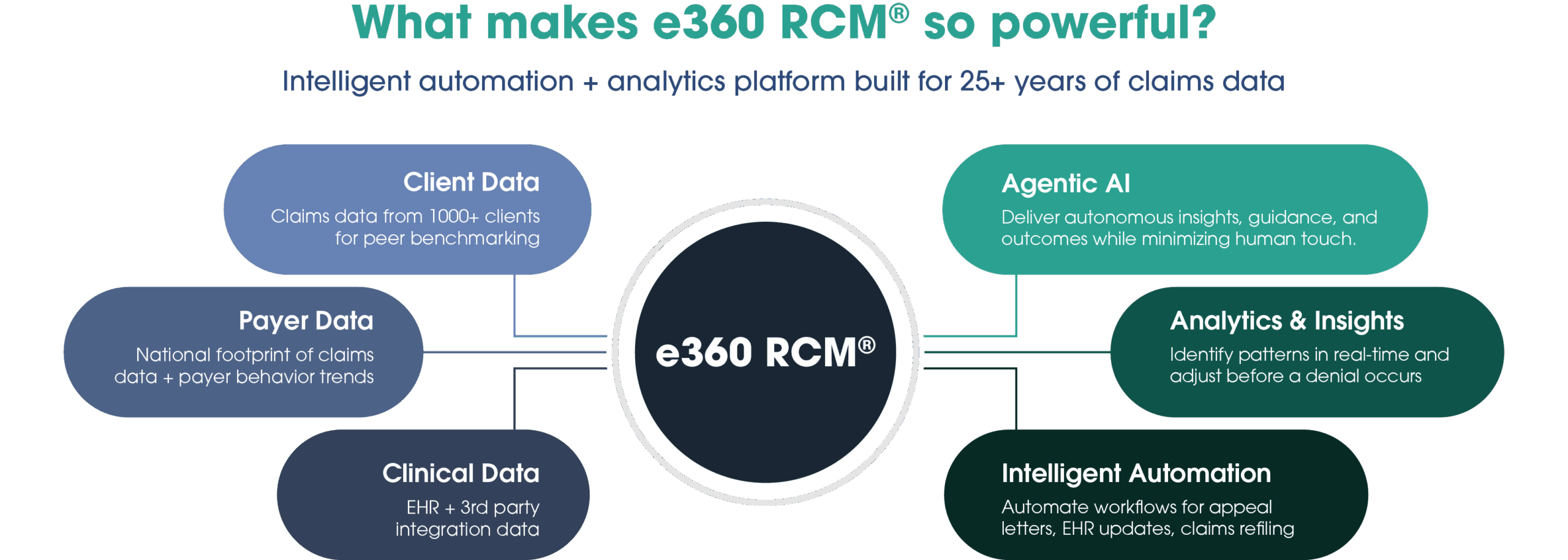
E360 isn’t just powered by AI – it's guided by intelligence.
Fusing AI technologies with hard-won insight, the platform examines every corner of the revenue cycle to maximize your financial performance. Our future-ready architecture is built for scale, governance, and predictive insights.
E360 gets smarter with every claim.
By applying rules-based automation, machine learning, and agentic AI, our technology platform gives providers an immediate and lasting revenue capture advantage.