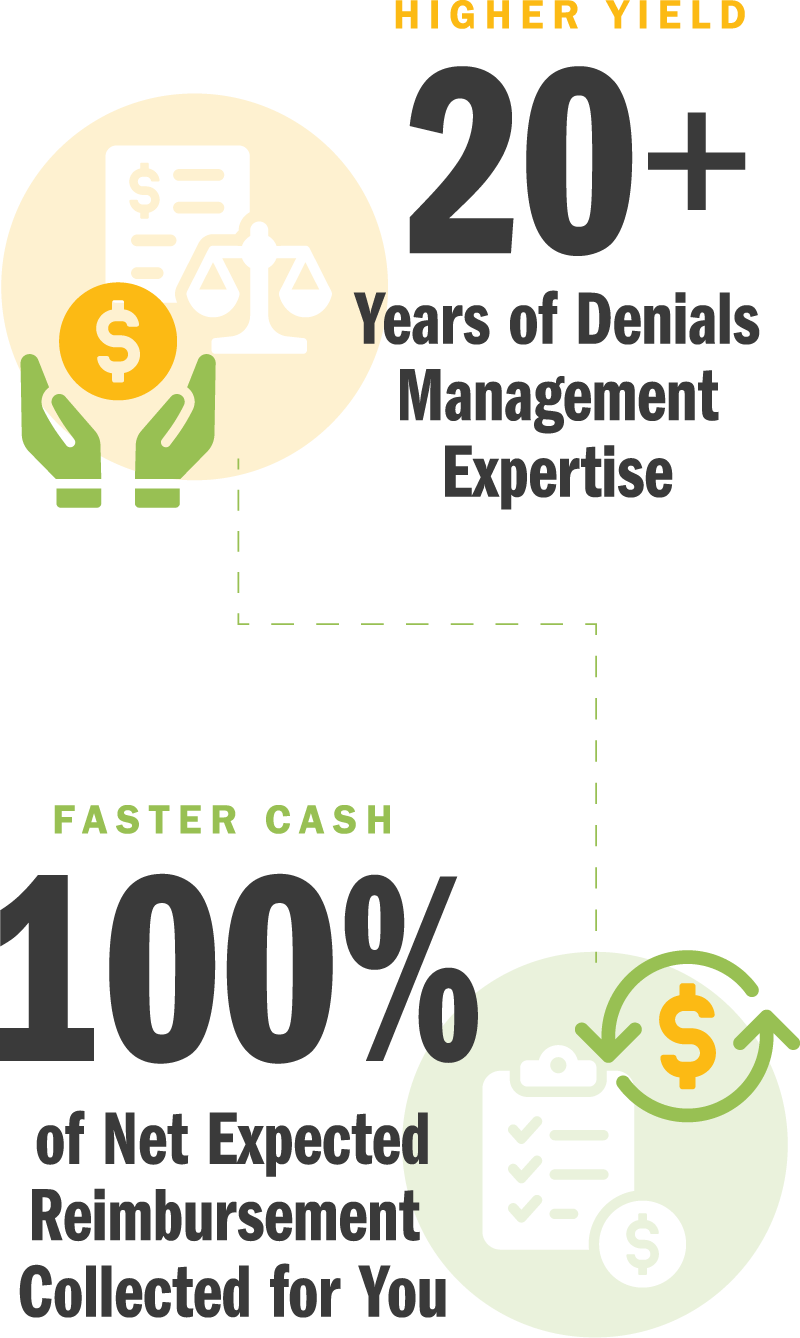
We identify and prevent denials — providing root-cause analysis and reworking even the most complex claims to enhance your revenue and yield.
Denials are one of the biggest challenges facing healthcare systems today. Managing and preventing denials is a complex and time-intensive process. Decentralized revenue cycle functions, manual workflows, and constantly changing payer policies make it incredibly difficult to address denials without specialized skill sets.
We are your “department down the hall” with the resources and skills to prevent and resolve your claim reimbursement denials — whether you’re a healthcare provider of one or a healthcare system of many.
We provide root-cause insights based on numerous complex coding and billing solutions by modeling various technical, administrative, and clinical data.
Our proprietary E360 RCM™ system allows for contract modeling to the most complex levels, providing an extremely comprehensive analysis of payment accuracy and integrity.
We provide specialized resources to resolve your most challenging accounts.
What you can do to reduce denials for your organization.
How to avoid denials from registration to reimbursement.
Denials can be time-consuming and frustrating, but you’re not alone.
Not sure if you’re leaving money on the table? We’ll conduct a high-level analysis of your open A/R, denials, and claims that are considered “closed” and carry a zero balance.
With your RevAdvise™ consultation, you’ll gain insight into your:
Looking for some quick wins? We’ll also show you how fast you can recover that revenue.
No cost. No obligation. No risk.






























Our contract is always contingent on your results.
You’re in good hands with our team of legal experts, healthcare professionals, revenue specialists, and technology experts.
Our E360 RCM™ platform interfaces directly and securely with your EHR/HRIS system.
With seamless integration and service, all you’ll see is the boost to your bottom line.