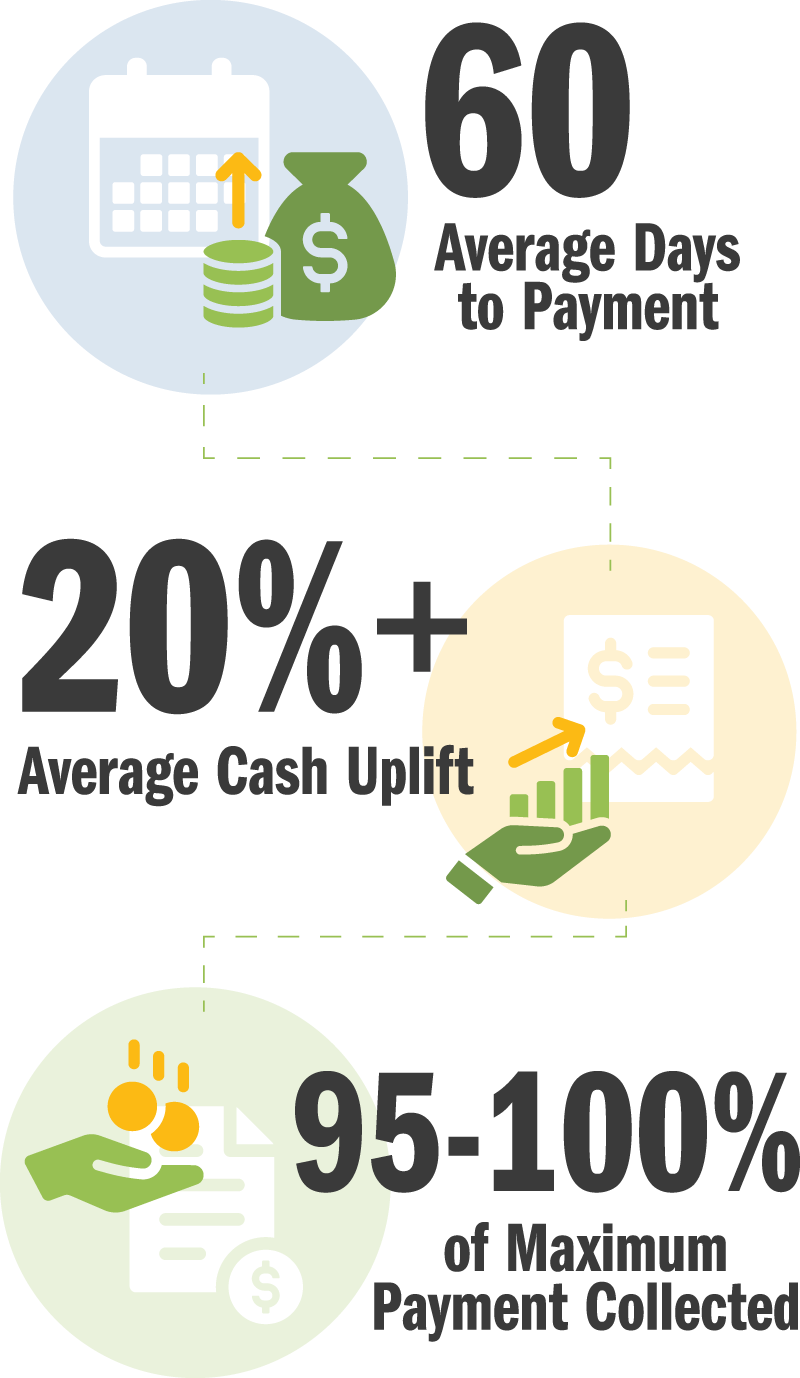
When you partner with EnableComp, you gain access to our industry-leading expertise and proprietary Intelligent Automation Platform so you can offload the workers’ compensation process and remove the burden of payment from patients and your institution.
The path to workers’ compensation reimbursement is littered with challenges that drain your resources and create more questions than answers.
We are your “department down the hall” with the resources and infrastructure to endure the workers’ compensation process and get the most out of your claims — whether you’re a healthcare provider of one or a healthcare system of many.
Our tenacious team of workers’ compensation experts apply their deep knowledge of state rules and dispute-resolution processes — including USDOL — to ensure successful cash recovery. Our relationships with the state hospital associations help protect or improve state workers’ compensation rules and avoid formal disputes with payers.
Our proprietary software platform, E360 RCM™, interfaces directly and securely with clearinghouses and your EHR/HRIS system — using RPA technology to automate workflows and ensure timely, accurate filing.
Our Managed Care Team works with your organization’s Managed Care department to review, negotiate, and advocate for optimal rates and reimbursements.
Our in-house team of nurses and clinical leaders review claims and associated documents as well as the payer denial or EOB and generate acceptable responses along with recommended next steps.
Our Certified Professional Coders (CPC) provide coding support to our revenue specialists and your team. When a claim is rejected because the code is wrong and the payer doesn’t say why, we do the research and scrub the claim so there are no issues.
We handle both hospital and physician-based workers’ compensation claims from registration to reimbursement. We have your workers’ compensation claims covered every step of the way.
Based on your organization’s priorities.
Proprietary Discovery Solution
We utilize extensive foundational intelligence to validate and confirm expected reimbursement.
Preparation
Automation-enhanced estimation and accuracy checks for required data and supporting documentation prior to sending to the payer.
Timely Filing
Bill is packaged and submitted electronically, when possible.
Follow-Up
Aggressive follow-up and process monitoring.
Status Documentation
Notes updated daily to ensure visibility into the status of every claim.
Payment Review
Underpaid items are identified automatically and appealed.
Denial Management
We pursue full reimbursement on your behalf and help fine-tune internal processes to prevent denials from recurring.
Appeals
We appeal when applicable as well as represent your hospital in subsequent matters when allowed.
Detailed monthly reporting based on pre-defined priorities to help you measure progress and reconcile accounts.
We identify state fee schedules and PPO-contractual adjustments to make sure you’re not overpaying or missing out on opportunities.
We take on old and new claims across the reimbursement lifecycle. Whether you choose to outsource some or all of your workers’ compensation claims, you get Intelligent Automation, seamless implementation, ongoing client engagement, and expertise that goes above and beyond.
A comprehensive solution that works all of your workers’ compensation claims from every angle for maximum impact and ROI. Ideal for providers who are ready to focus solely on higher-priority claim categories by outsourcing their workers’ compensation claims.
Your Day One Solution includes:
We start on day one and work claims from registration to reimbursement for consistently accurate and timely payments.
We inherit your open claims and manage aging accounts to a successful resolution for improved queue management and inventory reconciliation.
We help you negotiate the best rate possible and determine whether accepting a payer’s discount proposal is in your best interest.
We identify and prevent denials — providing root-cause analysis and reworking even the most complex claims to enhance revenue and yield.
We dig deep into claims that are considered “closed” and carry a zero balance to help you recover cash you’ve already written off.
Forecasts and strategies for healthcare providers.
Forecasts and strategies for healthcare providers.
Strategies for success.
Successful reimbursement begins at registration.
Confessions of a workers’ compensation payer.
Not sure if you’re leaving money on the table? We’ll conduct a high-level analysis of your open A/R, denials, and claims that are considered “closed” and carry a zero balance.
With your RevAdvise™ consultation, you’ll gain insight into your:
Looking for some quick wins? We’ll also show you how fast you can recover that revenue.
No cost. No obligation. No risk.






























Our contract is always contingent on your results.
You’re in good hands with our team of legal experts, healthcare professionals, revenue specialists, and technology experts.
Our E360 RCM™ platform interfaces directly and securely with your EHR/HRIS system.
With seamless integration and service, all you’ll see is the boost to your bottom line.